 3
|
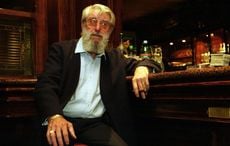
| Rory Staunton taking his first flying lesson in 2011. |
As many of our readers are aware my beloved nephew Rory Staunton passed away in NYU hospital from Toxic Shock Syndrome on April 1st.
I have written extensively about Rory and what happened to him but neither me or his parents, Ciaran and Orlaith Staunton, had any idea of just how a devastating series of events and mistakes cost him his life.
They occurred both with his primary care physician and in the NYU emergency room and doomed Rory’s chances of survival which should have been 100 percent with proper treatment.
Pulitzer Prize winner Jim Dwyer, a columnist with The New York Times, a close friend who knew Rory, launched his own investigative effort to determine the facts. What he discovered is carried today in The New York Times and has been the top rated story on their site.
It is a shocking story of medical malpractice in my opinion, and I only hope it can help other parents whose kids may face emergency room situations to learn from it. If Rory’s death can help save another child then it was not totally in vain.
Copyright The New York Times
“In a Boy’s Fight for his life , signs that went unheeded”
By Jim Dwyer
“For a moment, an emergency room doctor stepped away from the scrum of people working on Rory Staunton, 12, and spoke to his parents.
“Your son is seriously ill,” the doctor said.
“How seriously?” Rory’s mother, Orlaith Staunton, asked.
The doctor paused.
“Gravely ill,” he said.
How could that be?
Two days earlier, diving for a basketball at his school gym, Rory had cut his arm. He arrived at his pediatrician’s office the next day, Thursday, March 29,vomiting, feverish and with pain in his leg. He was sent to the emergency room at NYU Langone Medical Center. The doctors agreed: he was suffering from an upset stomach and dehydration. He was given fluids, told to take Tylenol, and sent home.
Partially camouflaged by ordinary childhood woes, Rory’s condition was, in fact, already dire. Bacteria had gotten into his blood, probably through the cut on his arm. He was sliding into a septic crisis, an avalanche of immune responses to infection from which he would not escape. On April 1, three nights after he was sent home from the emergency room, he died in the intensive care unit. The cause was severe septic shock brought on by the infection, hospital records say.
Because sepsis, a leading cause of death in hospitals, can at first look like less serious ailments, a campaign to aggressively identify it for early treatment has been undertaken by a consortium of 55 hospitals in the New York region, including NYU Langone.
Yet nowhere along Rory’s journey, from boy with a bellyache on Thursday to gravely ill boy on Friday night, did anyone act on strong indications that he might be fighting for his life. Critical information gathered by his family doctor and during his first visit to NYU Langone either was not used, was not at hand or was not viewed as important when decisions were made about his care, records show.
Moments after an emergency room doctor ordered Rory’s discharge believing fluids had made him better, his vital signs, recorded while still at the hospital, suggested that he could be seriously ill. Even more pointed signals emerged three hours later, when the Stauntons were at home: the hospital’s laboratory reported that Rory was producing vast quantities of cells that combat bacterial infection, a warning that sepsis could be on the horizon.
The Stauntons knew nothing of his weak vital signs or abnormal lab results.
“Nobody said anything that night,” Ms. Staunton said. “None of you followed up the next day on that kid, and he’s at home, dying on the couch?”
NYU Langone declined to discuss any aspects of Rory’s care or hospital procedures.
“Our deepest sympathies go out to the family at this difficult time,” said Lisa Greiner, a hospital spokeswoman.
The Stauntons shared Rory’s medical records with a reporter for The New York Times who had met the boy last summer in a social setting. A full airing of the case, along with a commitment to reforms, his parents said, could save lives. They have hired a lawyer, Thomas A. Moore, but have not decided how they will proceed.
Rory Staunton, 5 feet 9 inches tall and 169 pounds, was big for his age and a student of the world. “The most profound 12-year-old I had ever met,” his debate coach, Kevin Burgoyne, said. For his birthday, his parents gave him flying lessons after Rory, who spent hours on a flight simulator, tracked down an aviation school that accepted students at 12. He devoured the memoir of Chesley B. Sullenberger III, the pilot who safely brought down an airliner on the Hudson River.
“I told him, ‘Sully did some fast math landing that plane,’ and for a short while, he was paying attention to math,” said Ciaran Staunton, Rory’s father. “Then he came back with, ‘Yeah, but by the time I’m a pilot they’ll have a faster way of doing it.’ ”
Rory and his sister, Kathleen, 10, grew up in Sunnyside Gardens, Queens, which their parents, Irish immigrants, regarded as a global village of sublime pleasures: shared courtyards, a rich brew of cultures and merry mobs of children rolling from house to house. Ms. Staunton, the former director of an international student exchange, said neighborhood kids formed their own country, Kidadelphia, designed a flag, and adapted the United States motto for their slogan: “In God and Fun We Trust.” Rory was president. When he was 8, he raided his piggy bank to treat his parents to a Chinese dinner for their wedding anniversary. At the private Garden School in Jackson Heights, he was elected to the student council in seventh grade and led a campaign, Spread the Word to End the Word, to curtail the casual, derogatory use of the term “retarded.”
Last summer, his uncle, a friend of mine, brought Rory, Kathleen and their mother to stay in my family’s vacation home for two nights. Rory would go from barreling down a water slide backward to sizing up President Obama’s prospects for re-election. Fascinated by North Korea, he tried to fathom how a country so afflicted by famine could afford a large army. (His parents recently found a note in his computer to the Swedish ambassador to North Korea.)
At home, said Mr. Staunton, a civic activist and bar owner, they would have nightly shouting matches over homework Rory had not done or dirty clothes he had not picked up, in between scoping out corners of global history.
During gym class on Wednesday, March 28, he dived for a ball and opened a cut on his arm. That night, Ms. Staunton said, Rory mentioned it: “How he presented it to me was, ‘I fell in the gym. Mr. D, the athletic director, put the Band-Aids on. And, I got the ball.’ ”
Then he finished his homework and went to bed.
The bacteria Streptococcus pyogenes is part of the human ecosystem, normally dwelling in the throat or on the skin, areas where the body is well defended. Also known as Group A streptococcus, the strain typically causes strep throat or impetigo.
But if it is able to penetrate soft tissue or blood, “it moves very quickly,” said Dr. Michael B. Edmond, the chairman of the division of infectious diseases at Virginia Commonwealth University. “The mortality rate is high. The clinical findings early in the infection can be relatively subtle.”
The challenge for physicians is recognizing an invasive infection, whether from Group A strep or other pathogens, before the cascading damage of sepsis has picked up too much speed. The consortium of New York hospitals has a goal of starting antibioticswithin an hour of spotting sepsis in the emergency room, according to officials with the Greater New York Hospital Association’s Stop Sepsis program.
For every hour’s delay in giving antibiotics after very low blood pressure had set in, a large study found, the survival rate decreased by 7.6 percent.
Shortly after midnight on March 29, Ms. Staunton heard Rory retching in the bathroom. “There wasn’t a huge amount of vomit, but he kept saying, ‘My leg, my leg, Mom,’ ” she recalled. Back in bed, he moaned. His mother rubbed his thigh. In the morning, he was weak, his leg still hurt, and his temperature was 104 degrees, his highest ever.
The parents began calling Dr. Susan Levitzky, who had been the family pediatrician for about five years. She saw Rory that evening.
“He was leaning on me as we were walking up to the office, because he could hardly stand from the weakness or pain in his leg,” Ms. Staunton said. In the waiting room, Rory vomited. When the doctor swabbed his throat, he vomited on her. The swab test, a rapid but not definitive detector of strep, was negative.
“We showed her the cut on his elbow, and I saw her follow up his arm from the cut,” Ms. Staunton said. “She said, ‘The cut’s not an issue.’ She focused on his stomach. We said, ‘Although you see him throwing up, that’s not what he’s really complaining about.’ Rory and I both said to her that it’s the pain in his leg that’s really bothering him.”
The doctor told them that the leg pain might be from falling in the gym. “Rory said, ‘It wasn’t a fall, it was a skid,’ ” Ms. Staunton recalled.
The parents also remarked that Rory’s skin became blotchy when they pressed a finger on it. Those concerns were well-founded, said Dr. Edmond, the infectious disease specialist, who was not involved in Rory’s care: the mottling, which Dr. Levitzky made note of, could mean that vessels in his skin were constricting from low blood pressure; the leg pain could mean an invasive infection. Rory’s temperature was 102 and his pulse was 140; he was breathing 36 times a minute.
These, too, were “worrisome” observations, Dr. Edmond said.
Nevertheless, Ms. Staunton said, she did not recall being told that any of his vital signs were off: “She said, ‘Make your way over to NYU, and get him rehydrated. He’s vomiting now. He’s going to feel better, and tomorrow, he’ll have diarrhea.’ ”
In a brief phone conversation, Dr. Levitzky said she could not discuss the case. “I sent him to a major medical center,” she said.
Rory arrived at NYU Langone, on First Avenue near 34th Street, at 7:14 that evening and was discharged about two hours later. Hospital records do not reflect any communication with Dr. Levitzky or her findings about the mottled skin.
Like Dr. Levitzky, the NYU physicians believed that Rory’s discomfort was caused by a sick stomach and dehydration. His chart states that “labs, I.V.F., Zofran” were ordered.Zofran is an anti-nausea drug; two bags of intravenous fluids, or I.V.F., were administered; three vials of blood were drawn and sent to the hospital laboratory.
“They did the various checks, up, down, back and forth,” Mr. Staunton said.
A screening tool in the Stop Sepsis program, used when a patient first arrives in the emergency room, calls special attention to a person with three symptoms of a possible eight. At the hospital, Rory showed two: he was breathing 20 times per minute and his pulse was 143.
Two hours later, though, he had three: his temperature had risen to 102, his pulse was 131 and his respiration rate was 22. But by the time those vital signs were recorded, at 9:26 p.m., they had no bearing on his treatment. In fact, the doctor had already decided that Rory was going home. Rory’s “ExitCare” instructions, signed by his father, were printed 12 minutes before those readings.
To the pediatrician who examined and discharged Rory, it seemed that the fluids had done the trick. “Pt improved,” the doctor, Camille Scribner, wrote, prescribing “home supportive care.” There is no sign in the records that Dr. Scribner, described by a senior colleague as “hyper-conscientious,” considered alternative explanations.
“They stated that it was a common flu that was going around,” Mr. Staunton said. “It would start off as high temperature and throwing up, and would end up as diarrhea.”
Dr. Scribner could not be reached for comment through the hospital.
As the Stauntons walked Rory onto First Avenue, the air temperature was in the mid-40s. “He was freezing,” Ms. Staunton said. “He took my coat leaving the hospital. It has a little frilly thing around the collar.”
“Not a thing that a boy of 12 would put on,” Mr. Staunton said.
About three hours later, Rory’s lab results were printed. He was producing neutrophilsand bands, white blood cells, at rates that were “very abnormal and would suggest a serious bacterial infection,” Dr. Edmond said.
The Stauntons said they heard nothing about it. In bed, Rory “was groaning in his sleep,” Ms. Staunton said. “I felt the heat of the fever.”
At 10 a.m. on Friday, the Stauntons began calling their pediatrician, Dr. Levitzky. “She told us to do a combination of Tylenol and Motrin,” Ms. Staunton said.
Asked last month about the lab findings, Dr. Levitzky, who is associated with NYU Langone, said, “I never knew that testing was done.”
Rory did have the predicted bout of diarrhea on Friday, which momentarily elated his family. Still, he could barely get to the bathroom. The doctor suggested fluids and crackers.
“‘I told her, ‘I’m not sure you’re getting the picture, Dr. Levitzky,’ ” Mr. Staunton said. “‘I can’t even get him to sit up. I don’t know how you expect me to get food into him.’ ”
Later, a slight touch would make him scream. “Around his nose was gone blue,” Mr. Staunton said. “Down his body side was gone blue.”
At that point, Dr. Levitzky told them to return to the emergency room. They supported him as he walked to the car. “All he said was, ‘Can I please have a wheelchair when I get there?’ ” Ms. Staunton recalled.
In the intensive care unit, his parents tried to mask their worry, Mr. Staunton chatting lightly. But Ms. Staunton noticed her son’s eyes following her. “He said, ‘Mom, my toes are really, really cold,’ ” she said.
After extending an arm for blood to be drawn, “he thanked them when they were finished,” Ms. Staunton said.
He had to be put on a ventilator. Just before he was sedated, Ms. Staunton said, “They told him, ‘We need to figure some stuff out. There are some marks on your body, and you need a little bit of help breathing, so we’re just going to intubate you and it’ll be fine.’ ” First, though, they checked his mental status.
“Do you know what date it is?”
“I know it’s March,” Rory answered.
“Who’s the president of the United States?”
He answered: “Barack Obama.”
His mother smiled.
“Ah,” she said, “but Rory, who is going to be the next one?”
“Barack Obama,” he said.
As the next two days passed, doctors tried anything that might halt the shutdown of Rory’s organs. “I can’t say enough about the I.C.U.,” Ms. Staunton said.
Relatives and a priest gathered bedside, talking of Irish football and tomfoolery and politics. Perhaps, one doctor whispered in a fleeting, hopeful aside, Rory might get away with losing his toes and nose. His skin blackened. He passed no urine. His blood would not clot. His heart had to be restarted twice. Three specialists who chronicled Rory’s decline on his intensive care chart each noted that on Thursday night, when he was sent home from the emergency room, he had a fever and significant signs of infection in his blood.
On Sunday night, Dr. Mayer Sagy, who had not seen Rory on his first visit to the hospital but spent the weekend struggling to keep Rory alive, told the Stauntons that the team had been unable to resuscitate him a third time.
“I said to him, ‘I brought him here to you the other night and you sent him home,’ ” Ms. Staunton said.
“He said, ‘You have every right to be angry.’ ”
More than anything, the Stauntons said, NYU Langone owes an honest accounting of what happened.
Racked with loss, they and others remembered Rory as an unflinching champion of schoolyard underdogs.
“Above all,” Ms. Staunton said, “we know that Rory would want no other child to go through what he went through.”
For more information visit www.rorystaunton.com.



Comments